Most of the articles on UNstuck Nutrition focus on anti-inflammatory foods to try or how to implement an anti-inflammatory diet.
You may want to know when you will see the benefits of an anti-inflammatory diet.
How long will it take for the anti-inflammatory diet to work?
What improvements can you expect?
Let’s look at the chronic conditions associated with inflammation, ways to monitor inflammation levels, and how long it will take to see improvements.
Chronic Conditions Associated with Inflammation
Chronic conditions (also called non-communicable diseases) account for over 70% of worldwide deaths(1).
Chronic inflammation has been associated with these diet and age-related chronic conditions (2):
- type 2 diabetes or insulin resistance
- obesity
- heart disease
- stroke
- some cancers (colorectal, tobacco-related, kidney, ovarian, pancreatic, lung, mesothelioma, and prostate)
- asthma and COPD
- bone health (osteoarthritis, osteoporosis, and fractures)
- mental health, Alzheimer’s disease, and depression
- inflammatory bowel diseases (ulcerative colitis or Crohn’s)
- rheumatoid arthritis
- chronic kidney disease
- lupus, or scleroderma
The chronic condition itself can contribute to chronic inflammation, while lifestyle choices and diet can further exacerbate inflammation. An anti-inflammatory diet or lifestyle choice can prevent some chronic conditions. Other conditions can be improved or managed to enhance your quality of life.
Symptoms of Chronic Inflammation
Here are some common symptoms of chronic inflammation (2):
- body pain like joint or muscle pain
- chronic fatigue and insomnia
- depression, anxiety, and mood disorders
- gastrointestinal complications like increased constipation, diarrhea, and heartburn
- weight changes
- frequent infections or illnesses
- condition-specific symptoms (example: worsened asthma)
Tracking your symptoms related to your specific chronic condition(s) can help observe changes for the better or worse. For example, with type 2 diabetes, your blood sugar is likely higher when you are inflamed, whether from stress, poor sleep, or food choices.
Blood Testing for Inflammation
There is no one test to see if you have chronic inflammation. Typically, inflammation tests are done when monitoring a chronic medical condition and how you respond to diet, lifestyle, or medications (2).
Additionally, these tests will measure any type of inflammation (acute or chronic). The following two tests are considered good markers of chronic systemic inflammation. Remember that the number may be elevated if you have had a recent illness or injury.
Inexpensive and Effective Blood Tests:
- high-sensitivity C-reactive protein (CRP)
- fibrinogen
The following markers of inflammation are measured in some research studies and with certain medical conditions. These tests are expensive and specific, generally looking for pro-inflammatory markers:
- tumor necrosis factor-alpha (TNF-alpha)
- interleukin-1 beta (IL-1beta)
- interleukin-6 (IL-6)
- interleukin-8 (IL-8)
Inflammation levels are not tested routinely. Your regular medical care assesses the status of conditions that cause chronic inflammation. Research has shown that excess weight (especially in the abdominal area), type 2 diabetes, and heart disease are linked to chronic inflammation(1,2).
Your healthcare provider generally does not need to test if you have inflammation if you have warning signs like physical inactivity, low fruit and vegetable intake, weight gain, or less-than-ideal insulin, blood sugar, or lipid levels. They know you have chronic inflammation.
Tracking Inflammation and Progress
Instead of testing, a better plan is to make lifestyle changes, add more anti-inflammatory foods, and manage any chronic conditions contributing to inflammation. Track progress before making changes and along the way. Self-monitoring is a motivating and free tool!
What Should You Track?
Deciding what to track is more individualized. Evaluate your current status.
I like to put a number on it, ranking from 1 (going poorly) to 10 (doing great). The ranking is not a perfect science, but it is more to see improvement as you make changes.
You can also track how often symptoms occur. Is it once daily? Several times per day? As you make changes, the frequency of symptoms should decrease.
Here are some areas you could track:
- energy level
- pain (pick areas that most affect you)
- GI issues (constipation, diarrhea, heartburn severity and frequency)
- how often do you get sick, and how long do you stay sick?
- quality sleep (ideally 7 to 9 hours)
- headaches (severity and frequency)
- blood sugar levels
How Should You Keep Track?
Some people like to track on paper or a hard copy calendar. Others like to use the calendar or notes feature on their phone to monitor their ranking, frequency, and severity of symptoms. You can even use smartwatches to track changes.
I recommend tracking daily at the beginning. After adjusting your day to take time to assess your body and symptoms, you will create a habit and do this automatically. But you may not need to notate the information as frequently as you will be more in tune with your body.
My Fitbit tracks my physical activity, sleep, and heart rate. I have been monitoring since Christmas 2014 and can predict how my body responds accurately.
If my sleep is poor for several days in a row, my heart rate trends up, and I know my chronic conditions might flare up that week. That tends to show up as headaches, tiredness, and more likely to get colds or illnesses. My mood and energy levels are also lower if I haven’t been physically active.
Why Should You Track?
Tracking your symptoms related to inflammation, healthy lifestyle, and chronic conditions will help you know how your body responds.
It will help you prioritize certain things because you feel better when you sleep well, exercise, and eat nourishing anti-inflammatory foods.
Tracking motivates you to keep going and making small changes.
What’s better than no change? A small change. What’s better than a small change? Several small changes over time which in time make a transformative impact.
It took a long time to be in your present nutrition/inflammatory/health state, and it will take purposeful, small daily changes to change the direction of your nutrition and health. You are on a journey to better health.
A line graph is one of my favorite ways to illustrate nutrition change over time.
We WANT the line to be perfectly straight and improving. And this is what diets and quick fixes unrealistically promise!
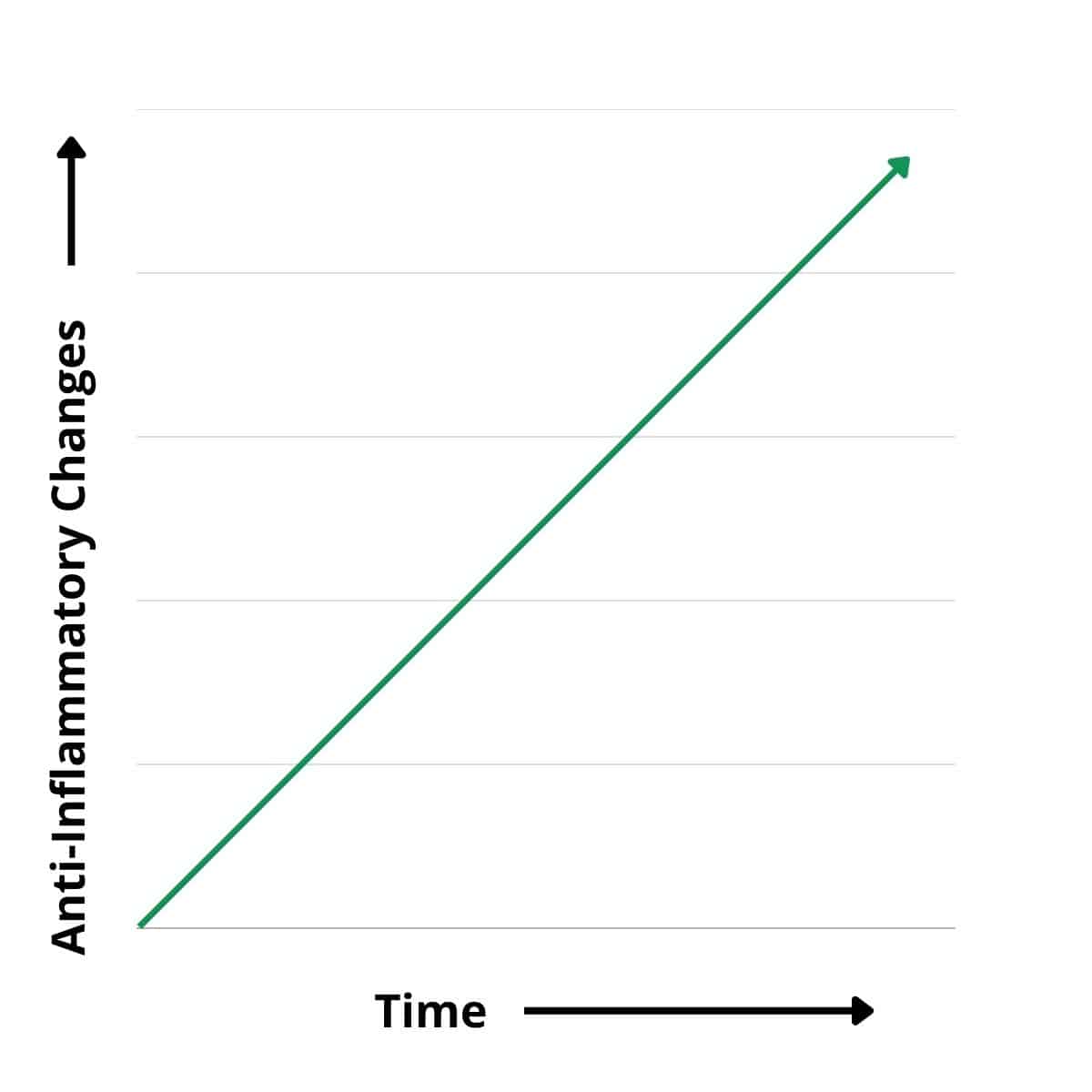
But in reality, we will have ups and downs (normal and expected) as we incorporate healthier lifestyle habits. The crooked line is an accurate picture of change in our lives. These downs are just one part of the picture and are temporary.
Sometimes, we focus on the red circle, and it feels like we are failing and want to give up entirely.
Zoom out and remember all the changes you have made and can make again. Tracking helps you see this progress!
You can keep pressing forward and making one small change! You learned how to change in the past, and you are reading this article, which is evidence of a small change you made to improve your life. Your body (and brain) know how to do that again, even in a lapse.
How Long Will It Take For the Anti-inflammatory Diet to Work?
You may notice improvements like increased energy or feeling full longer after meals in the first week. However, it may take up to 12 weeks to see differences in lab levels or drastic improvements in chronic conditions.
Most clinical trials and research studies have participants follow an anti-inflammatory diet or include anti-inflammatory foods for at least 12 weeks. However, most take significantly longer to look for strong relationships. Twelve weeks is about how long it can take to see meaningful changes in your lipid, insulin, and glucose levels.
Here is a snapshot of short-term and long-term results after an anti-inflammatory diet.
I searched for studies with a 12-week or less time frame following an anti-inflammatory diet. I included extensive, long-term studies with solid evidence supporting the anti-inflammatory diet.
Type 2 Diabetes
Long Term Effects:
| Study | Results |
| A meta-analysis with 122,810 individuals were divided into groups of low, medium, or high adherence to the Mediterranean Diet and followed the participants for 3 to 20 years. This meta-analysis included data from the PREDIMED Study listed below. | High adherence to the Mediterranean Diet was associated with a 19% lower risk of developing type 2 diabetes (3). The Mediterranean diet reduces HbA1c by 0.32 to 0.53% (3). |
| The ATTICA Study compared dietary habits among 3,042 adults and those with and without diabetes, along with follow-ups at 5, 10, and 20 years after the start in 2001 and 2002. | Those with a higher score of Mediterranean Diet adherence had a 15% lower fasting glucose and insulin and 27% lower insulin resistance (4). |
Short-Term Effects
| Study | Results |
| Nineteen people with type 2 diabetes followed the anti-inflammatory Mediterranean Diet, including three fruit servings daily for 12 weeks, and then switched to a non-Mediterranean Diet. | Flavonoid (antioxidant) levels increased by 50%, the diet reduced inflammatory marker IL-6 by 49%, and a stress marker by 32% (5). |
| Forty people with pre-diabetes or type 2 diabetes were assigned 12 weeks of the Mediterranean Diet and then 12 weeks of the ketogenic diet. Researchers measured lab results after 12 weeks on each diet. | HbA1c and weight decreased similarly for both diets, LDL cholesterol decreased with the Mediterranean Diet, and HDL cholesterol improved for both diets. The researchers found much lower intakes of fiber and nutrients on the ketogenic diet. The follow-up data from participants revealed they preferred following the Mediterranean Diet as it was more sustainable and realistic (6). |
| Twenty-seven participants with type 2 diabetes consumed their usual diet for 12 weeks or a Mediterranean Diet for 12 weeks and then crossed over to the alternate diet. | HbA1c fell from 7.1% to 6.8% with the Mediterranean Diet. Plant food intake increased by four times their average. Antioxidant levels increased by over 25% while saturated and trans-fat levels decreased. Monounsaturated fat or heart-healthy fats increased (7). |
Heart Disease
| Study | Results |
| The PREDIMED Study followed 7,447 people at high risk for heart disease for almost five years. The participants were randomly assigned one of three diets: a Mediterranean Diet with 1 liter of extra virgin olive oil a week, a Mediterranean Diet with ¼ cup of nuts daily, or a low-fat diet. | Both Mediterranean Diets offered a 30% reduction in heart events (heart attack, stroke, or death). The Mediterranean Diet improved blood pressure, insulin sensitivity, lipid levels, inflammation, oxidative stress, and artery plaque build-up. The PREDIMED Study proved that the anti-inflammatory Mediterranean Diet (full of vegetables, unsaturated fats, and flavonoids) prevents heart disease (8). |
| Researchers used the ATTICA study to look at the effect of the Mediterranean diet on total antioxidant capacity (TAC) in 3042 adults with no heart disease. | TAC was 11% higher in those adhering most to the Mediterranean Diet compared to the lowest adherence. LDL cholesterol levels were 19% lower in the highest-ranked diet group. High TAC was related directly to increased olive oil, fruit, and vegetable intake (9). |
Knee Osteoarthritis
| Study | Results |
| Knee osteoarthritis (KOA) is a common problem, especially when carrying extra weight. Researchers wanted to investigate whether dietary components improved pain without achieving weight loss. 129 patients with KOA were randomized to their regular diet, a low-fat diet, or a Mediterranean Diet for 12 weeks. | Both the low-fat and Mediterranean diet participants lost similar amounts of weight. Pain was significantly decreased in the Mediterranean Diet compared to the low-fat and regular diet. Compared to the regular diet, physical function improved with the Mediterranean diet. The dietary components of the Mediterranean Diet help reduce pain, regardless of weight loss (10). |
Age-Related Cognitive Decline
| Study | Results |
| The PREDIMED trial data was looked at from several angles. Researchers looked at 447 cognitively healthy older adults (average age of 67 years) with neuropsychological baseline and end-of-study assessments. Patients were randomly assigned a Mediterranean Diet with 1 liter of extra virgin olive oil a week, a Mediterranean Diet supplemented with ¼ cup of nuts, or a low-fat diet. | After four years of the assigned diet, cognitive assessments were analyzed in 334 participants. A Mediterranean Diet supplemented with olive oil or nuts was associated with improved cognitive performance (including auditory verbal learning, memory, attention, working memory, language, and processing speed). The beneficial effect of the Mediterranean Diet on cognition is likely from the anti-inflammatory nature of fruits, vegetables, extra virgin olive oil, and nuts. Oxidative processes can harm the brain if not counteracted with antioxidants found in many foods on the Mediterranean Diet (11). |
Childhood Chronic Conditions
Non-Alcoholic Fatty Liver Disease (NAFLD)
| Study | Results |
| NAFLD is becoming more common in children due to increasing rates of obesity, diabetes, and insulin resistance. Treatment involves diet and lifestyle changes to reduce liver fat and normalize elevated liver enzymes. Researchers placed children with NAFLD aged 9-17 years old on a Mediterranean Diet or a low-fat diet for 12 weeks. The Mediterranean Diet is not low-fat but focuses on choosing heart-healthy fats. | Liver fat decreased along with liver enzymes for both groups. Insulin resistance improved more on the Mediterranean Diet. No significant decrease in calorie intake was required, allowing for adequate childhood growth (12). |
Childhood Asthma
| Study | Results |
| Researchers looked at the effects of the Mediterranean Diet on 104 children with childhood asthma (aged 1-5 years). The children were enrolled in a one-year program and compared data from before and after starting the Mediterranean Diet. | 32.2% of children had no asthma attacks, 35.3% only had one attack, and 24.9% had two attacks. The children averaged 4.73 asthma attacks the previous year. Inhaled corticosteroids decreased from 3.92 to 1.09 times per patient per year. Inhaled bronchodilators decreased from 4.14 to 1.12 times per patient per year. The families involved in the study reported high satisfaction with improved asthma control and following a Mediterranean Diet (13). |
Colds and Ear Infections
| Study | Results |
| Two recent studies (2016 and 2022) have linked a child’s diet to a pro-inflammatory state, predisposing them to recurrent colds and ear infections. The 2016 study focused primarily on cold frequency in 128 children (average age of 2.9 years old) adopting the Mediterranean Diet over one year. | Before the study and following the Mediterranean Diet, the children averaged 7.45 colds per year and afterward averaged 2.88 colds yearly. Inflammatory complications were reduced from 4.64 to 0.7 episodes. Antibiotic use was reduced from 3.85 times per patient per year to 0.49 times (14). |
| The second study, released by the same authors, focused on ear infections in the same age group (1 to 5 years old) among 90 children. The children’s diets were high in animal-based products and processed foods. They also hypothesized that the mucosa (tissue lining) in the whole ear, nose, and throat area is pro-inflammatory and hyper-reactive due to the inadequate diet. | By the end of the year-long anti-inflammatory diet implementation: No patients could meet the criteria for recurrent ear infections. 60% of the patients had no further ear infections. Ear infection occurrences dropped from 3.84 to 0.48. Pain intensity during the ear infections dropped from 1.6 to 0.09. Antibiotic use dropped from 4.3 times per patient per year to 0.66. Family satisfaction and adherence to the Mediterranean Diet were high (15). |
Takeaways
Chronic conditions contribute to inflammation. Diet and lifestyle changes can reduce inflammation.
Tracking your inflammation symptoms while adopting an anti-inflammatory diet and lifestyle can motivate you to make small, impactful changes.
The Mediterranean Diet is a flexible anti-inflammatory eating plan that can be followed for life compared to more restrictive diets (ketogenic or low-fat).
A restrictive diet may work short-term but often leads to burnout, a reversal of previous unhealthy eating habits, and undoing the positive benefits you have accomplished.
Research on anti-inflammatory diets shows improvements within 12 weeks for various chronic conditions across all ages. Long-term research shows a strong association between improved health conditions and an anti-inflammatory diet.
You can read more of my research-based articles with simple tips for adding more anti-inflammatory foods and drinks to your diet.